By Dr Claire Steves
Our healthcare system faces myriad challenges in the next fifty years. We’ve been aware of our growing elderly population for many years, but so far little has been done to address the challenges this raises for the future of healthcare. Here, Dr Claire Steves lays out her vision of healthcare, and what we can do now to prevent current challenges becoming serious problems in the future.
This blog has been adapted from Claire’s speech at The King’s Fund’s Festival of Ideas event on 6th October 2017.
When asked to think about a way forward for healthcare, I think it’s first helpful to look back through the history of medicine. I like to think of medical history in three eras: the preservative, the diagnostic, and hopefully, in the future, the integrated era.
The first era of medicine: preservative
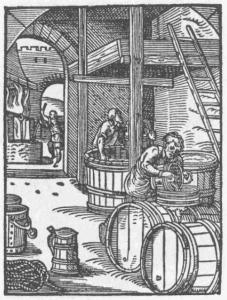
The premedical “preservative” era extends back for millennia. This era represents the majority of human history when the main health threats were starvation, and infection. Strategies that humans created then have had huge implications for human health now. Most important has been the use preservatives to avoid infection, and keep food and water fresh.
Our main healthcare resources to combat infection in the preservative era were salt for preserving meat, alcohol for fruit and most importantly water (if you had a liking for fermented products, you were much less likely to die of cholera!), and sugar, which was not only a preservative but also a valuable energy source. Our ancestors who chose these foods may have had a selective advantage, but that advantage is gone today.
Perhaps driven by this need to conserve energy, as adults we appear to have an increasing tendency to move as little as possible. As a mother of three boys, I’m intrigued that children have such an insatiable desire to move, and yet this seems to disappear as we age; with adult humans choosing energy conservation and sedentary lives.
Could it be that this preventative medicine and tendency to over eat and conserve energy means that we are programmed to prefer things that are no longer beneficial?
So, healthcare in the premedical, preservative era was preventative, practiced in the home by housewives and mothers. In industrial times, city planners became important, introducing water systems which improved sanitation. Then followed widespread use of antibiotics, the magic bullet of the 20th century. These two revolutions have contributed to the increase in our lifespan over the last 100 years.
“…over indulgence and a preference for moving as little as possible have impacts for healthcare”
But all medicine has side effects. The preservative era has left us with hangovers which we are still feeling today; over indulgence and a preference for moving as little as possible have impacts for healthcare. Emerging evidence that antibiotics have changed the microbes in our guts, with effects on a wide range of chronic conditions, suggests that even our medicines can leave us with new problems. These hangovers have particular relevance now that we are living much longer, and evidence suggests that these fractors are driving unhealthy ageing.
The second era of medicine: diagnostic
The healthcare service we have today has been built on the second era of medicine. I call this the era of the “unifying diagnosis”. This has been an era where we have honed the classification, diagnosis and treatment of specific diseases.
The massive advances in medicine have targeted single diseases or conditions and have been hugely successful in preventing and treating these diseases. The hospital has, for the most part been the central hub, and scientists, doctors and nurses have put the medicine into practice and the more specialised and focused the better.
These two eras of medicine – the preservative and the unifying diagnosis – have led to an increase in life expectancy, which has rocketed especially in the last 150 years. The slightly less good news, however, is that the average man now spends 16 years at the end of his life with functional limitation, and the average woman 19 years!
This means that sort of medicine costing the most, and with the biggest burden within our services has now changed. The main users of healthcare have also changed. The biggest burden of ill health is now shouldered by the oldest among us, and these people are not well served by the “unifying diagnotic” model.
“The biggest burden of ill health is now shouldered by the oldest among us, and these people are not well served by the [current] medical model”
The unsolved problem we are now facing has been called many names, most of them problematic: frailty, multimorbidity, Geriatric Giants. One thing is for sure, it’s no longer about ‘diagnosed cases’ and ‘controls’, but more about sliding scales with age. I particularly like the word “homeostenosis”.
Many of us are familiar with homeostasis – the ability to keep things in balance. Homeostenosis on the other hand is gradual reduction in the ability to keep things in balance, to the point where equilibrium is disturbed and the ability to function is lost. This process happens on multiple levels – physiologically, psychologically and socially.
So has the success of the unifying-diagnostic model of medicine, of diagnosis and treatment of specific diseases, revealed the problem that was laid down in the preservative pre-medical era? It seems that the institutions built during the diagnostic era don’t seem to be providing solutions which work. We need to ask ourselves: is our health service built to help people with multiple needs on multiple levels? This is what we need to focus on to reverse the side effects of our medical history.
“…is our health service built to help people with multiple needs on multiple levels?”
We need to restructure our medical thinking, and move our services away from the “unifying diagnosis” and centralised healthcare. We also need to counter those things that are driving the phenomenon of frailty: caloric over indulgence, a preference for moving as little as possible, and, probably, excessive antibiotic use. We must aim our research at understanding and avoiding homeostenosis.
Immediate challenges
In my view, we have three key challenges to overcome in the near future to ensure that healthcare meets the demands of the future:
We need to change how we research the ageing process
A great deal has been invested in studying ageing using animal models, with the worm C. elegans, the fruit fly Drosophila, and the mouse having been put to great use in studying ageing, particularly lifespan. All three have highlighted insulin signalling pathways, and energy restriction as key to ageing. Mice have been very useful in showing the effects of physical activity. But animal models can only get us so far; they have perhaps been less helpful in studying the effects of alcohol and salt. These may be particular human problems!
Recently, there have been really exciting advances in animal research. Microbiota transplantation experiments in gnotobiotic mice, bred in sterile conditions with no gut microbes, are helping us to understand how our microbes may affect multiple physiologies simultaneously.
Despite these advances, there are two problems. Firstly, it’s not all about age, or living longer. We really should be focusing our efforts on maximising the amount of time we can live in good health, without frailty. To do this, animal models need to address the quality of ageing, not the quantity. Secondly, clinicians need to be directly involved in ageing research. Cardiology and cancer made their huge advances by ensuring that every consultant clinician had a research degree. In Geriatric Medicine (the biggest medical specialty) only 1 in 50 senior trainees have a research degree, and very few medical schools have a professor of Geriatric Medicine. This must change.
We need to encourage older adults to take part in research
It’s very difficult to engage and recruit frail older people in research. There are challenges with access to the research environment and there are risks associated with using interventions in those who are frail.
For example, I am involved in a multicentre study of two promising new treatments for sarcopenia – muscle wasting with ageing. We’re finding it almost impossible to recruit patients yet we urgently need to do the research to help translate geroscience – the study of the relationship between aging and age-related diseases – into the real world.
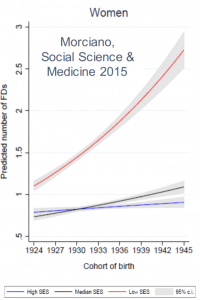
We need to address the social divides in ageing
There is a worrying divide where frail ageing is happening much more to the less well off. The functional difficulties associated with ageing are much more of a problem in the lowest socio-economic groups. And this is a problem that is getting worse, not better. We must ensure that any solutions we create reverse this health injustice.
All this is taking shape within a larger unsettled political landscape. Our health service and our research capability are being heavily threatened by our divorce from the European Union. This threat overshadows potential progress over the next fifty years, which we should not be shy of debating.
What are the assets at our disposal as we move to integrated healthcare?
If there is a poly pill, we already know what it is. There is already one clear key to health happiness and resilience: physical activity. But how do we get the whole population moving and remove our addiction to the combustion engine?
The information revolution means the structure of society no longer needs to focus on urban centres. Commuting no longer needs to dominate, and we can free up time for physical activity. Could we envisage a world where miles are minimised and foot travel is the preferred of interacting with our environment?
“If there is a poly pill, we already know what it is… physical activity”
For this to work physical activity needs to be both the most pleasant and most efficient way of doing things, both in work and in leisure, and must be embedded in every aspect of policy planning. We need to prioritise physical activity everywhere, from buildings to public spaces, from homes to offices. We also need physical activity to thrive in schools – it must be part of our way of life early on.
The second asset we have at our fingertips is the potential of personalised medicine. Here I’m talking about the possibility that we can use multi-omic technology, such as genomics, metabolomics, and metagenomics to provide medicine and prevention plans tailored to individuals.
For ageing, imagine that a person at that moment in their lives, perhaps at 40 or 50, when they start to realise that they are not invincible, that mortality will come also to them, and that perhaps they need to make some changes. Imagine they could have a series of tests that could show them how they are likely to age, and how that could change if they were to make some targeted lifestyle changes. Could this empower and motivate personal change?
This approach has huge potential, but we need to ensure that we do not widen existing health inequalities and that access to personalised medicine is available to everyone and anyone.
“…we need to ensure that … access to personalised medicine is available to everyone and anyone”
Our third potential asset is one we could use to reduce health injustice, or increase it. Social networks and big data are emerging as important fields of health research. Could we use these networks to target health education to reduce the health-economic divide?
If we can join social network “case finding” with personalised medicine using remote technologies, such as wearable tech and blood spot cards sent to doctors by post, we could imagine an entirely different world of preventative medicine. Social media is already being used by industry to target individuals – we’ve all seen personalised adverts on our computer screens. Can we do it in the NHS for the benefit of people’s health?
So where do we go from here?
Our lifespan is growing, in excess of our health span and the healthcare system we need to solve this issue is not the one we have come to rely on. We need to build translational ageing research, engage older adults in research, and counter the increasing health inequalities with age. Here I’ve outlined three key assets we can use to address these challenges: physical activity, personalised medicine and social networks. The time has come to use these assets to shape the healthcare system of the future. The third era of medicine must, like the first be an era of preventative medicine, but this time with fewer side effects!